At-home abortions are putting women's health at risk

Across England and Wales, three in every four abortions - or 75% - are now performed by women at home using abortion pills.
The Department of Health and Social Care (DHSC) recently reported a 17% increase in the number of abortions: a total of 123,219 in the first six months of 2022. The DHSC says that it is currently reviewing its systems for recording and reporting abortion complications, noting that for abortions at home, complications are not likely to be recorded.
Medical abortion (MA) involves taking two different medications. The first is called mifepristone – this blocks progesterone, the hormone needed for the continued development of the embryo – and it also prepares the body for the next medication.
After waiting 24 to 48 hours the second medication, misoprostol, is taken. This causes the softening and opening of the cervix and contractions of the uterus so that the dead embryo and placenta can be expelled through the vagina.
Up until the end of 2018, MA was one of the methods used by providers in abortion facilities. Women were required to attend in-person to take both medications, two days apart. Women attending for the misoprostol would only have been discharged by the providers after a careful clinical assessment to ensure that the abortion was complete.
When the medical abortion treatment fails, further medical intervention is required to remove any retained parts of the embryo and/or placenta to control bleeding and to prevent infection.
On 27 December 2018, the DHSC gave approval for women to self-administer the second treatment, misoprostol, at home after having taken the mifepristone at an abortion facility. On 30 March 2020, as an emergency response to Covid-19, the DHSC gave approval for both medications to be self-administered by women at home. This temporary approval was made permanent from 30 August 2022.
In the first six months of 2022, across England and Wales there was a total of 123,219 abortions - 675 every day.
Some 92,159 women self-managed their abortions at home, about 72% taking both medications and 28% self-administering the misoprostol at home after taking the mifepristone at an abortion facility. This means that on average, 505 women were self-managing their abortions at home, every day, seven days a week.
As noted above, this is a 17% increase over the same period in 2021. It is worth noting that both BPAS and MSI Reproductive Choices have stated a continued increasing trend into 2023; MSI-RC reports a 30% year-on-year increase in demand for abortion over the first five months in 2023.
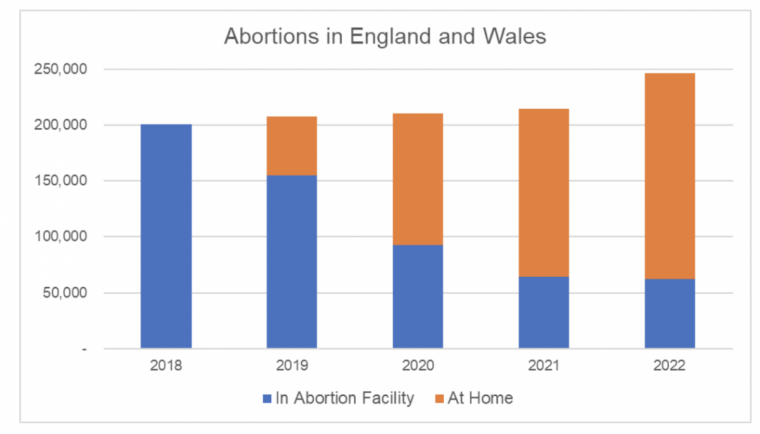
The above graph illustrates the growing proportion of abortions that are self-managed by women at home. The bar for 2022 extrapolates the data from the first six months to the full-year, on a flat-line basis, with no increase. Given the statement from MSI Reproductive Choices about a continued increase into 2023, this is a conservative estimate.
In 2018, there were 200,608 abortions performed at facilities across England and Wales, none at home. In 2022, we estimate a total of 246,000 abortions, 75% of which (184,000) were self-managed by women at home.
A critical issue of concern about these at-home abortions is the absence of any clinical assessments or aftercare; it really is all up to the woman herself. She must determine if her abortion has been completed and if not, she is now the one responsible for seeking further medical intervention.
This is a very unwelcome development in the provision of abortion services - the passing of clinical responsibility from the providers contracted and paid by the NHS, to the woman herself.
The DHSC states that complications were reported, using the HSA4 forms, in 161 out of 123,219 abortions in January to June 2022, a complications rate of 0.26%.
This is broadly in line with the numbers reported in previous years but as the DHSC says, these data on complications should be treated with caution. The HSA4 forms are usually completed and submitted to the DHSC by providers as soon as the abortion pills have been given to or posted to the woman; before the treatment is used and thus before any complications arise. The DHSC says for at-home abortions, complications are less likely to be recorded.
We previously investigated the rate of complications arising from medical abortion treatment failure. This table summarises the findings of our full report.
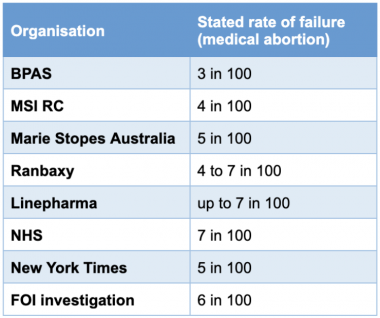
The medical abortion failure rate reported by Marie Stopes Australia in 2020 was 5%, meaning that one in 20 of women being treated with abortion pills in its facilities needed additional medical intervention to address complications arising from an incomplete abortion.
This rate is at the lower end of the estimated ranges from Ranbaxy and Linepharma, the manufacturers of the abortion pills used by providers in England and Wales. Five per cent is broadly consistent with findings from a detailed investigation by the New York Times and our own FOI Investigation across the NHS hospitals here.
What this means is that at least one in 20 of those women who self-manage their abortion at home will suffer complications arising from treatment failure. These women will need to seek medical help, usually at their local NHS hospital, or continue to suffer ongoing bleeding and risk infection.
Using the published DHSC data up to June 2022 and extrapolating on a flat-line basis to the end of June 2023, we estimate the following:
Since the beginning of 2019, across England and Wales, at least 590,000 women have self-managed their abortions at home. Assuming a treatment failure rate of 5%, as reported by Marie Stopes, 29,000 women will have suffered complications and needed medical intervention at their local NHS hospital.
Given the continued increasing numbers of abortions managed in this way, we can conservatively estimate that there are now 25 women needing hospital intervention every day because of failed medical abortion at home. Our estimate indicates as many as 4,600 complications in the same period in which the DHSC reported just 161; a huge difference by a multiple of almost 30x.
This could perhaps be described as an unintended consequence of the changes in abortion regulations that permit abortions by telephone, pills-by-post, and self-management of abortion by women at home.
Many are now calling for this to be ended and for a return to a required in-person consultation before the abortion treatment is given, for mandated follow-up by providers with women using the abortion pills at home, and of course for comprehensive reporting of complications data.
If nothing else, then surely women deserve to be told that there is at least a one in 20 risk that their medical abortion will fail and that they will consequently need hospital treatment. Otherwise, how can they give "informed consent"?
Kevin Duffy is a former Global Director of Clinics Development at Marie Stopes International and now a pro-life advocate.











